Pitfalls in Diagnosis of Shunt Malfunction in Children
DOI:
https://doi.org/10.5530/bems.9.2.6Keywords:
Shunt, Hydrocephalus, Intracranial pressure, Shunt malfunctionAbstract
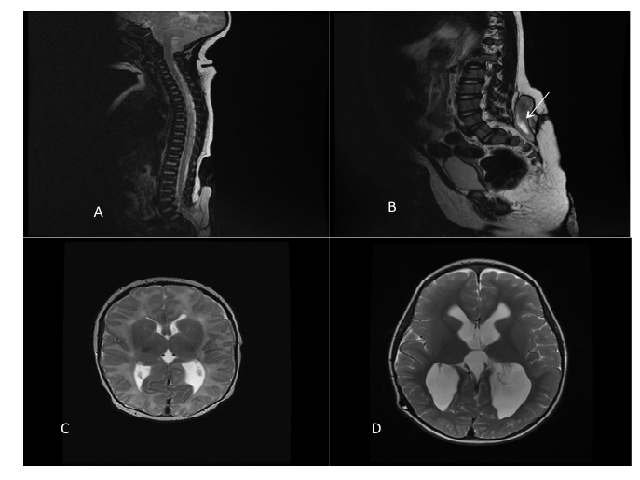
Background: In children with a potential shunt malfunction, pediatricians and emergency physicians are often the first to assess these children prior to neurosurgical referral. Most shunts fail within the first year (67%), with 14% of children having a shunt failure within the first month of insertion, and 40% within the second year of insertion. Classical symptoms of raised ICP, such as nausea, vomiting, coma and bulging fontanelle have a high predictive value for shunt failure, but are not always present. Some patients may be asymptomatic of shunt failure and the age of the patient will also confound this symptom spectrum. Clinical signs of shunt failure are well varied and age dependent. This article presents a series of four cases of shunted patients with atypical presentations of shunt malfunction. Materials and Methods: Clinical, radiological and surgical data of the patients were collected to demonstrate atypical presentations of shunt malfunction. All shunt malfunctions were confirmed upon review of the shunt in the operating theatre. Results: Four patients are shown to have atypical presentations of shunt malfunction. The first child was completely well despite an incidental finding of papilloedema on routine follow up, despite the lack of clinical and radiological evidence for shunt malfunction. The second child was completely well with a minor intermittent CSF leak at the drain wound. The third was an expanding pseudomeningocele after tumor resection. The final child had an expanding lower back pseudomeningocele but was otherwise well. All patients had resulting successful shunt revisions. Conclusion: It is important for neurosurgeons, paediatricians and emergency doctors to be able to identify these atypically presenting children and to correct their shunt malfunction to prevent long-term complications of insidious raised ICP, such as blindness or worsening of pre-existing neurological deficits and more importantly to prevent the child having a rapid and devastating decompensation.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Biology, Engineering, Medicine and Science Reports

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.